In the mid 1970s, I was fresh out of my surgical residency and ready to take on obesity with surgical interventions. Remember, my father had suddenly died from obesity and hypertension just a few years earlier.
As a surgeon, I had been trained to take a mechanistic approach to obesity. To our way of thinking, instead of helping people deal with their biology and environment, we should drastically reduce the number of calories that could be absorbed. We did this by reducing the usually 20 feet of small bowel to a mere foot and a half.
This procedure worked for many people, but many others suffered from malnutrition. For others, the shortened small intestine left too much bile and gastric acids to pass through the large bowel. From there, it would pass quickly through the rectum, not a comfortable situation. People had diarrhea, gas, and very raw and painful rectums.
I remember my first bypass patient, Bob. He was about 5’6” and weighed 360 pounds. His obesity was so severe that he could not sleep lying down and still breathe. So he had to sit in a chair and lean forward, propping his arms and head on a pillow placed, ironically, on the top of a small refrigerator. Worse, he was a smoker, and he often went to sleep in this position while smoking. His arms were covered from burns caused by lighted cigarettes falling from his mouth as he drifted off to sleep.
He was desperate, and I was a new surgeon, ready to save people with what I’d learned in my surgical residency training. Bob received a state-of-the-art small-bowel bypass. Initially, he recovered well. Bob did lose weight in the coming weeks but the diarrhea, gas, and painful rectal inflammation were more than he could take.
Bob was so miserable that at his six-month check-up, he pleaded with me to reconnect his small intestines. For him, the cure was worse than the disease. So I reversed his small bowel bypass. Unfortunately, I lost track of Bob. I will never know the final results of his surgical journey.
With such issues and problems, surgeons began trying other methods. For instance, we experimented with placing a row of staples across the top of the stomach, then we would remove one or two of them to create a small hole that allowed food to flow into the lower stomach. While mechanically this method made sense, very few people had long-term success with it. Their stomachs quickly stretched out, and patients learned it was a lot easier to drink milkshakes than to eat solid, healthy foods. As physicians, we did not yet understand the brain mechanisms that drove hunger and naively thought that people just needed to have more “willpower.” Once we’d shrunk their stomachs, we expected them to eat small, healthy meals.
During the 1980s, European surgeons popularized the “adjustable gastric band.” This procedure amounted to an elastic fluid filled balloon that wrapped around the upper part of the stomach. The band had a small tube which was attached to a reservoir that was placed on the abdominal wall, just under the skin. As the patient began to lose weight, the collar could be inflated by placing more saline liquid into the reservoir with a needle and syringe. This tightened the band and restricted the amount of food that could get into the stomach. Of course, if the band was too tight, people couldn’t even drink water.
Here in the United Sates, the gastric band procedure became very popular. It was a relatively simple procedure and often resulted in a 20 to 30 percent weight loss. But later we would learn that the procedure did not change the brain biology. People still craved food. These cravings were made worse because they could only get down a half a cup of food. So people would, once again, turn to milkshakes and sodas to get the calories they were craving.
Another problem arose. Because the procedure was so simple, almost any abdominal surgeon had the skill to place this simple device. Since medical insurance usually did not cover this procedure, many less scrupulous surgeons were charging high prices and gave little attention to the post-operative care. Despite these problems, I still see patients who have kept off 50 to 70 pounds, and they are healthier than before the procedure.
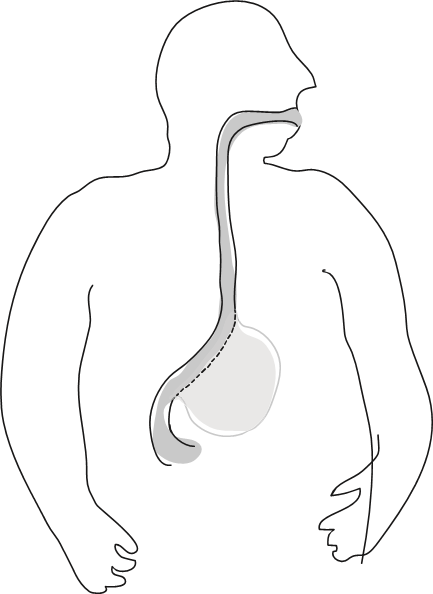
Fortunately, during the late 1990s and early 2000s, many academic research centers were beginning to do laboratory work and animal studies to better understand why some of us overeat, become obese, and cannot seem to lose weight. Two major therapeutic concepts began to take form. The first was called “restrictive” surgical methods similar to the gastric band. A current example of this method would be the gastric sleeve. This procedure is done laparoscopically and while under anesthesia, a sizing device is placed down through the mouth into the stomach. Using a stapling and cutting device, two rows of staples are then placed to divide the shorter inner curve of the stomach from the larger outer curve. This larger portion is then removed. What remains is a small “banana like” stomach.
People undergoing this procedure typically experience 65 to 75 percent reduction in “excess body weight.” The term “excess body weight” was created by the surgical community establishing the “ideal” body mass index (BMI) at 25, and then subtracting this weight from the person’s current weight. It has proven to be a useful standard, but is confusingly different from the term “percentage of weight lost” used by the medical bariatric world.
The outer curve of the stomach that is removed from the body is where the majority of the hunger hormone ghrelin is produced. Thus, patients who have had the gastric sleeve procedure will notice a significant decrease in food cravings. Unfortunately, this “no hunger honeymoon” only lasts for 12 to 24 months. While cravings, hunger, and a lack of fullness may return, these symptoms will never be as bad as before surgery. During this critical period of time after bariatric surgery, it is especially important for the patient to maintain a relationship with a provider who understands the biology of obesity and will follow them “forever”. This is when the use of anti-obesity medications may be needed again to counter the emerging “biology” changes of the hind brain.
Even before the “sleeve procedure” became established in the bariatric surgery quest for a solution to the “heavy biology” problem, surgeons were taking another look at the “malabsorption” methods I had been taught during my surgical training. Researchers asked if there could be a safer method that wouldn’t have all the previous side effects. The conclusion was that they might be able to combine both restrictive and malabsorption approaches. This “gold standard” of bariatric surgery is known as the Rou-en-Y gastric bypass. Essentially, this is a belt and suspenders method.
First, it creates a small gastric pouch just where the esophagus joins the stomach. This small pouch holds about two tablespoons, and is completely separated from the remainder of the stomach. The rest of the stomach will never be touched by food again, but it will remain in the abdomen to make gastric secretions.
Because food does not enter the main stomach remnant, ghrelin isn’t secreted. So like the gastric sleeve procedure, those going through Rou-en-Y gastric bypass will also have a reduction in cravings for 12 to 24 months.
About 18 inches after the small bowel has left the lower outlet of the stomach, the surgeon divides a section of the small bowel. The distal, or downstream, end is re-attached to the stomach pouch. The proximal, or upstream end, of the divided small bowel is re-attached to the side of the pouch limb about 31 to 59 inches below the stomach pouch. This creates the “Y” of Rou-en-Y. Now the bile, pancreatic, and gastric juices can start the digestive process, but up to 59 inches of small bowel absorption has been bypassed.
The total effect of this procedure is that the patient eats less food due to the thumb size gastric pouch, and less of the small bowel is absorbing calories, thus creating a degree of malabsorption.
This procedure has achieved dominance in the surgical communities around the world. The usual weight loss has been between 75 to 85 percent of excess body weight.
The gastric bypass and the gastric sleeve have become standardized due to the efforts of the American Society for Metabolic and Bariatric Surgery (ASMBA). Also, the safety of these procedures increased by establishing the designation of “Centers of Excellence” for hospitals with low levels of complications, and that had surgeons who demonstrated core competencies.
Bariatric surgeries are laparoscopic procedures. This means that the entire surgery is done through a series of small half inch incisions. The surgical instruments are passed into the abdomen through these incisions and the procedure is conducted by the surgeons manipulating and monitoring their surgical activities through screens positioned in the operating room
These efforts and advanced technology have reduced mortality for bariatric surgery from 1 percent down to 0.01 percent. These bariatric surgical procedures are now safer than having your gallbladder removed or your hip replaced. This is a far cry from the original small bowel bypass procedures that I did in the 1970s!
The safety and long-term success of our current bariatric surgery procedures has caused the insurance industry to take a second look at bariatric surgery. Currently, most medical insurance companies will cover the cost of the procedure. While we might think that this decision was out of the goodness of their hearts, covering bariatric surgery made good business sense. Early in the experience with the Rou-en-Y procedure, there was the unexpected discovery that patients with type 2 diabetes frequently found that their disease went into remission within three to ten days! This serendipitous finding has led significant research about the relationship between the bypass and certain “gut hormones” that influence insulin resistance.
For insurance companies, this remission of type 2 diabetes means significant medical cost savings. If an obese patient has type 2 diabetes and has bariatric surgery, especially the Rou-en-Y procedure, the cost of the surgery is “budget neutral” after two years because of the reduction in hospital admissions and medication costs.
The FDA established weight criteria for the use of anti-obesity medications but it was the medical insurance industry that established the weight criteria for bariatric surgery. A patient would qualify for bariatric surgery if they had a BMI greater than 40. They may also be approved for surgery if their BMI is greater than 35 and they have the comorbidities of diabetes, sleep apnea, hypertension or cardiovascular disease. Currently, there is no age restriction for bariatric surgery with most insurance companies.
With relatively minimal risk, people having bariatric surgery will experience health benefits well beyond the reduction in weight. With just the remission of type 2 diabetes, a person will not experience a wide range of secondary diseases such as kidney failure, coronary artery disease, diseases of the blood vessels in the lower limbs, and loss of eyesight and so on. This is why bariatric surgery leads to an 89 % increase in life expectancy and a decrease in the risk of dying from cancer by 60 percent.
Yes, there are some disadvantages to bariatric surgery; it is a surgical procedure after all. There are the usual risks of wound infection, blood clots to the lungs, and anesthesia complications. There can be non-lethal leaks at the staple lines where the digestive track is cut and reconnected.
But when you compare the advantages of bariatric surgery against the health destructive impact of the obesity Clash, surgery may be the better choice. While surgery may be an aggressive accommodation, it has now been proven to be the most effective and permanent method that we currently have.